If you've ever spent time in a Neonatal Intensive Care Unit (NICU) then you understand when someone describes it as a roller coaster. That is exactly what it is - whether your baby is in the NICU for 1 day or 1 year.
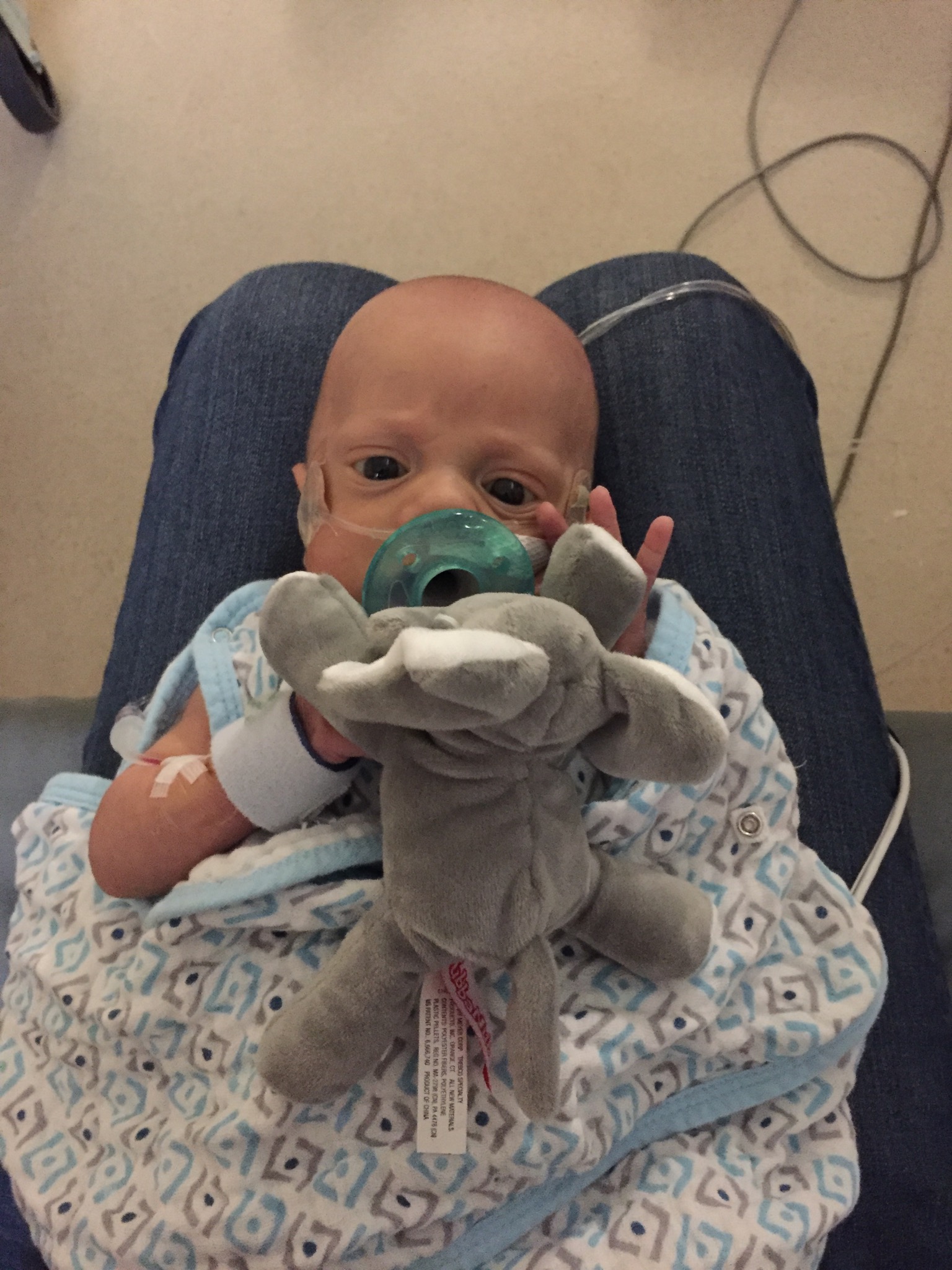
To give you some perspective on Conner's size - he is holding on to a MINI beanie baby.
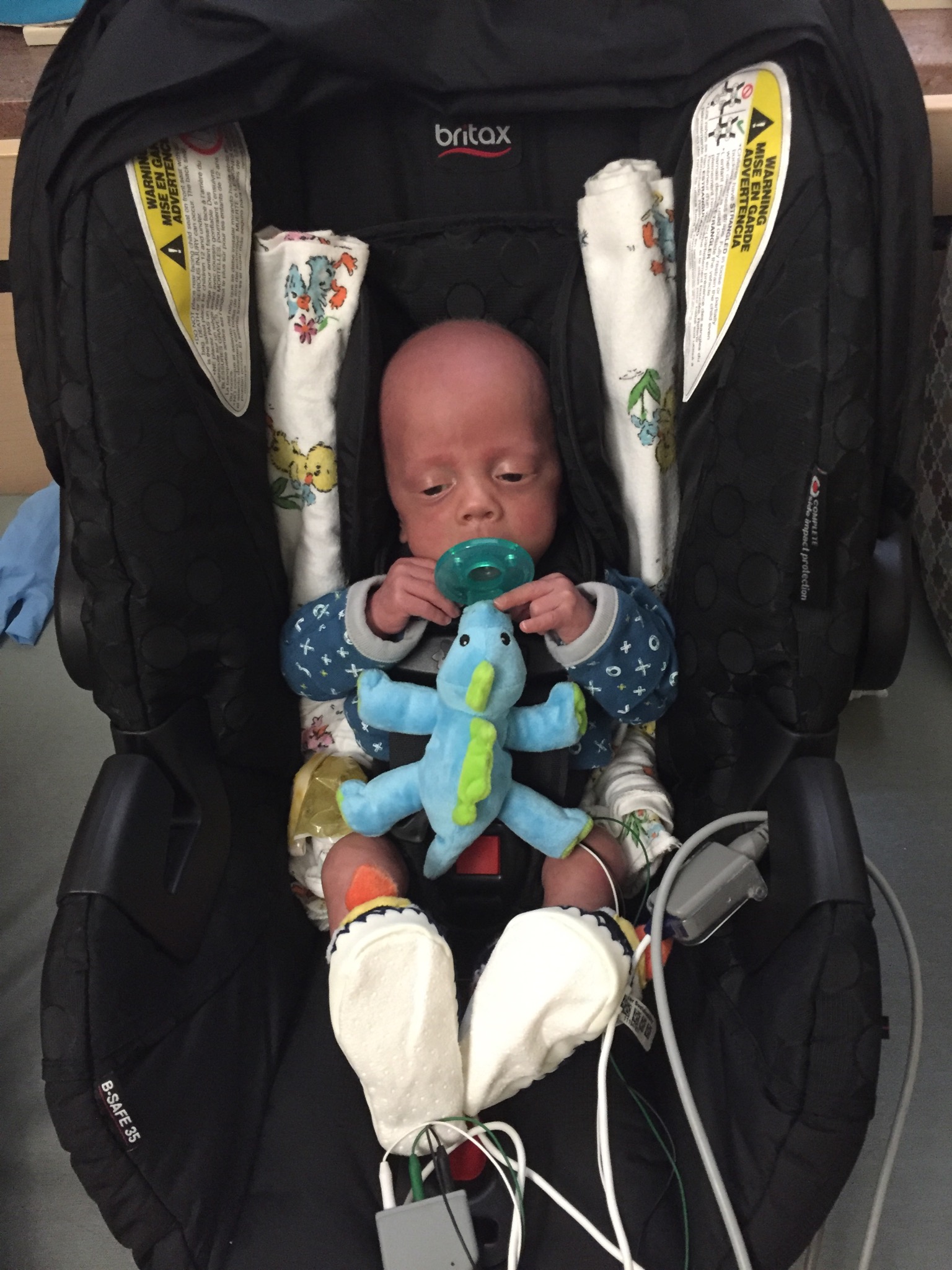
Conner spent 6.5 months, 194 days, 4,656 hours, 279,360 minutes, 16,761,600 seconds in two NICUs before he was strong enough to finally come home. Conner’s first 6 weeks of life began in the Children’s Hospital where he was born. However, they did not have a surgeon on call the night Conner became very ill with a suspected case of Necrotizing Enterocolitis (NEC), so he was transferred to another NICU in town. We then spent the remaining 5 months there. We had every kind of day possible and every emotion you can fathom - often both ends of the spectrum in the same day. Caring for a micro preemie in the NICU is like a teeter toter. Nothing comes without a price and Conner paid the price often.
Holding 2lb baby Conner for the first time
at 42 days old!
Terrified and thrilled beyond measure!
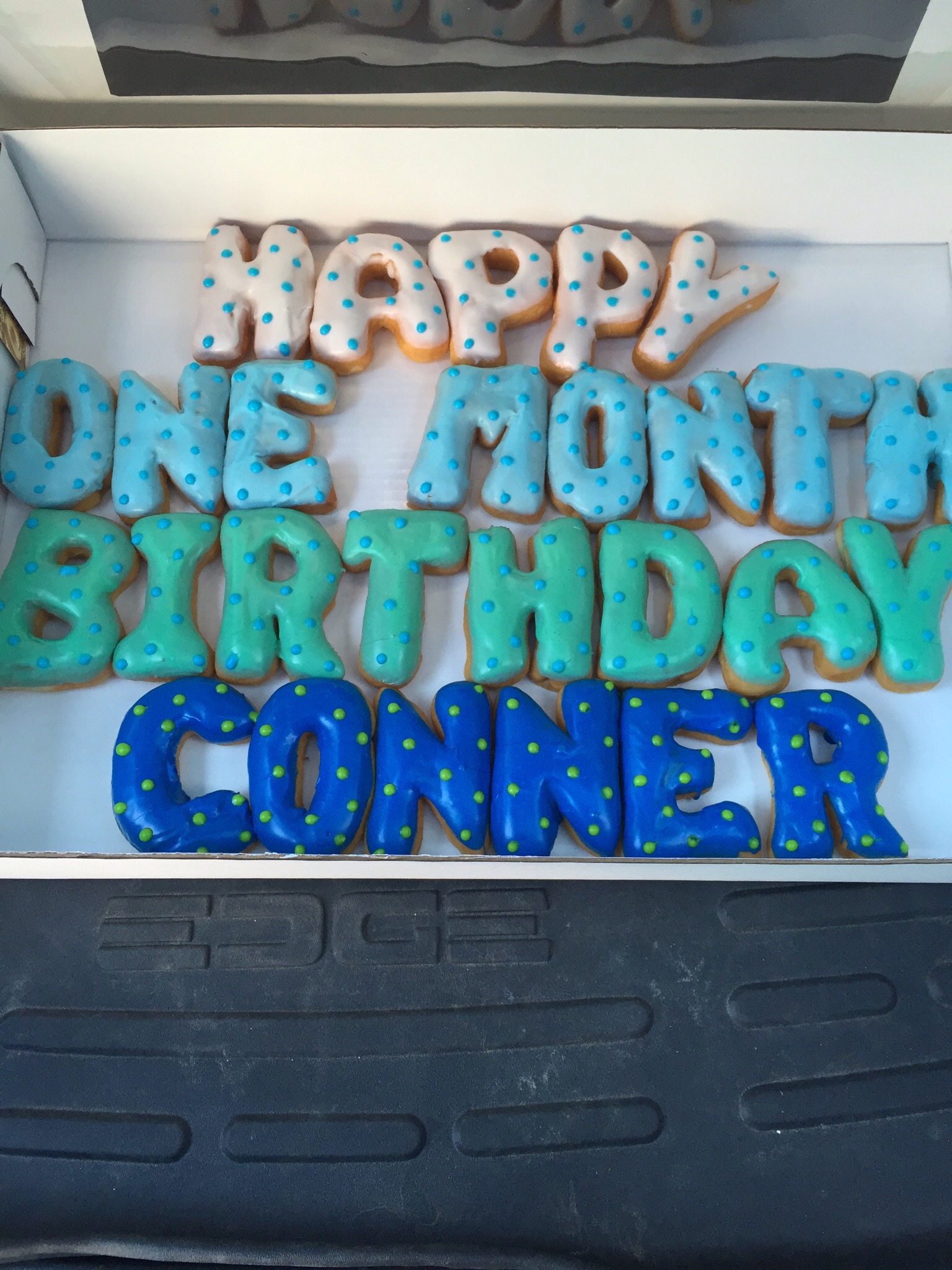
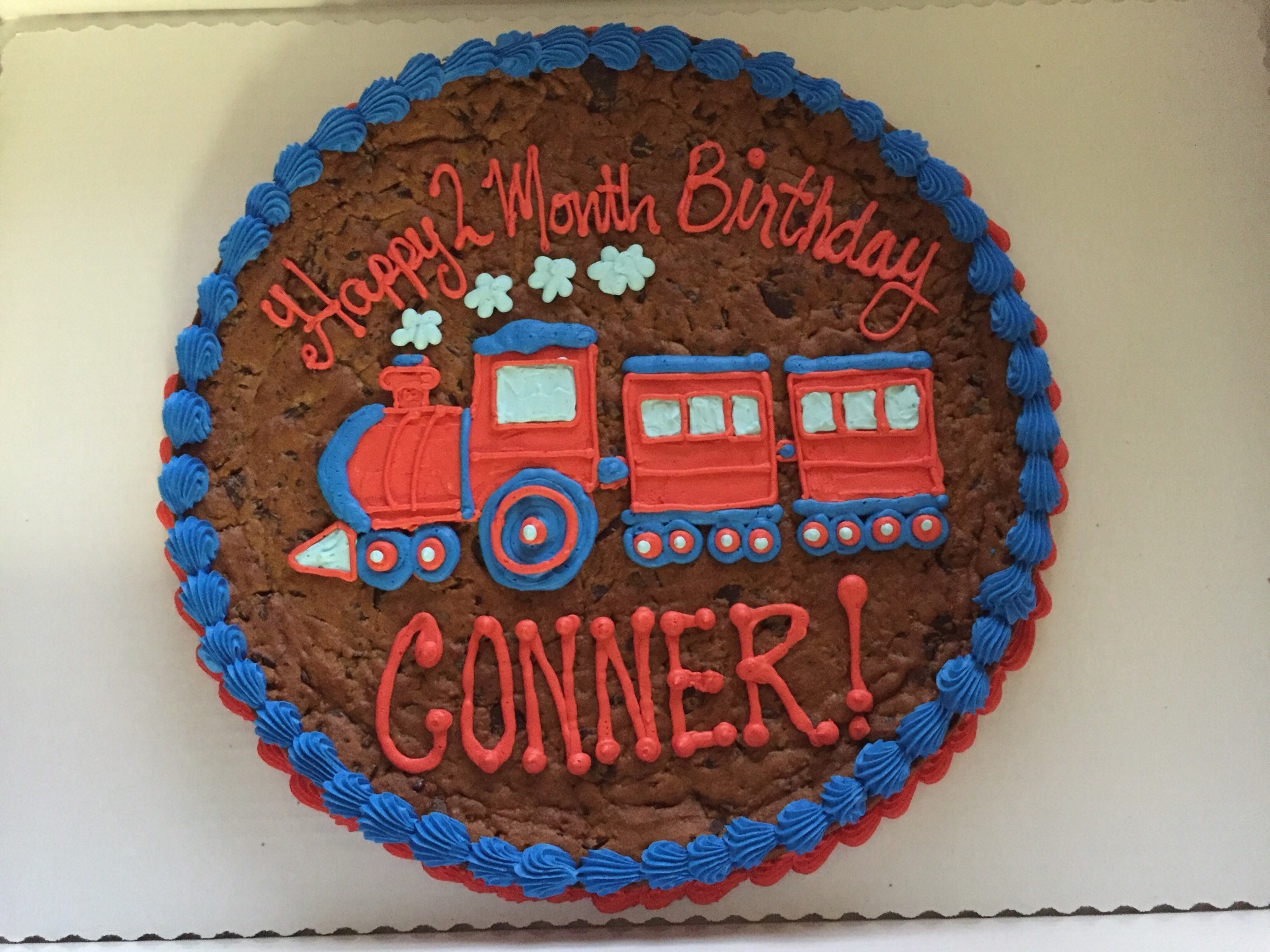
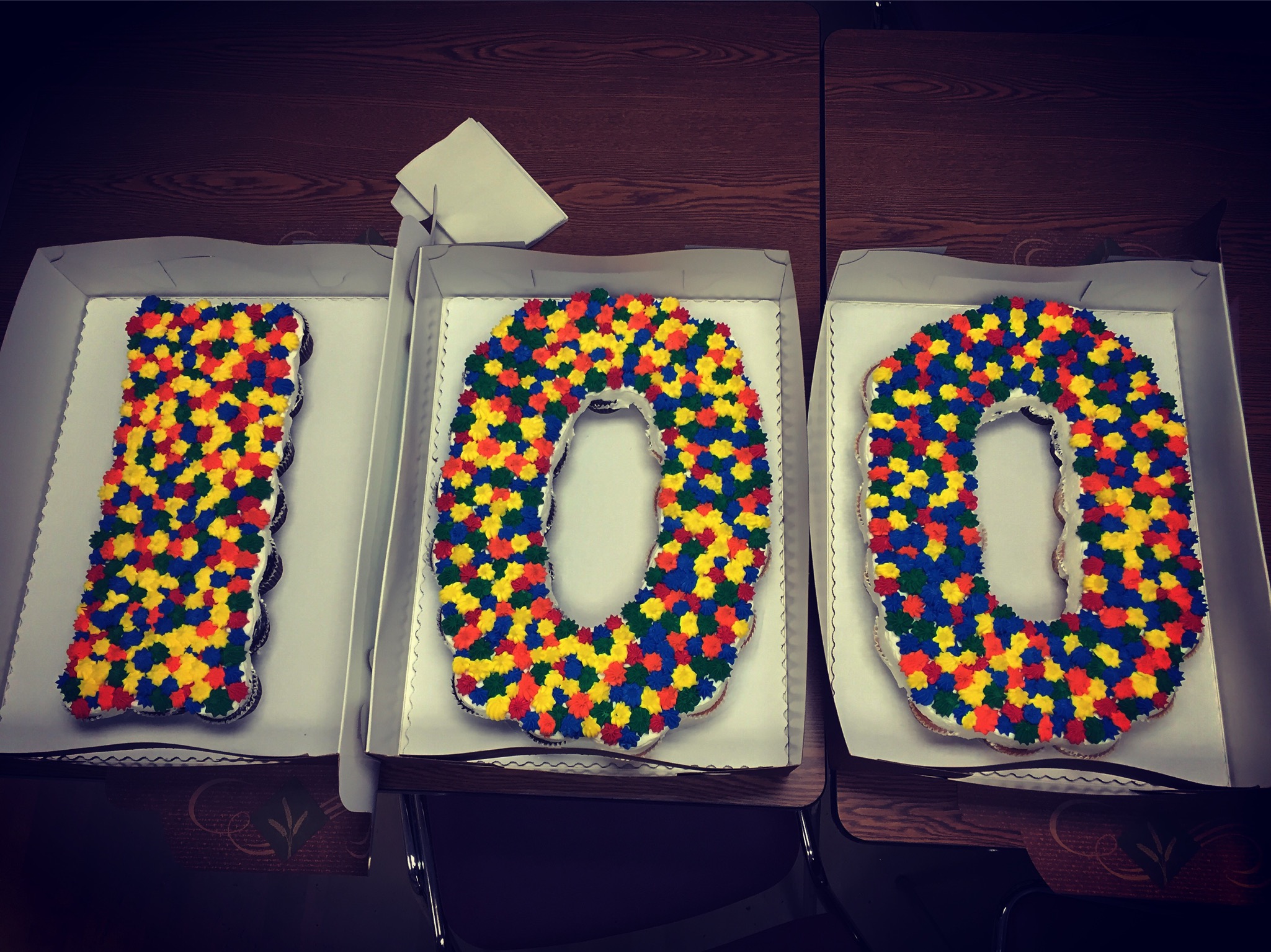
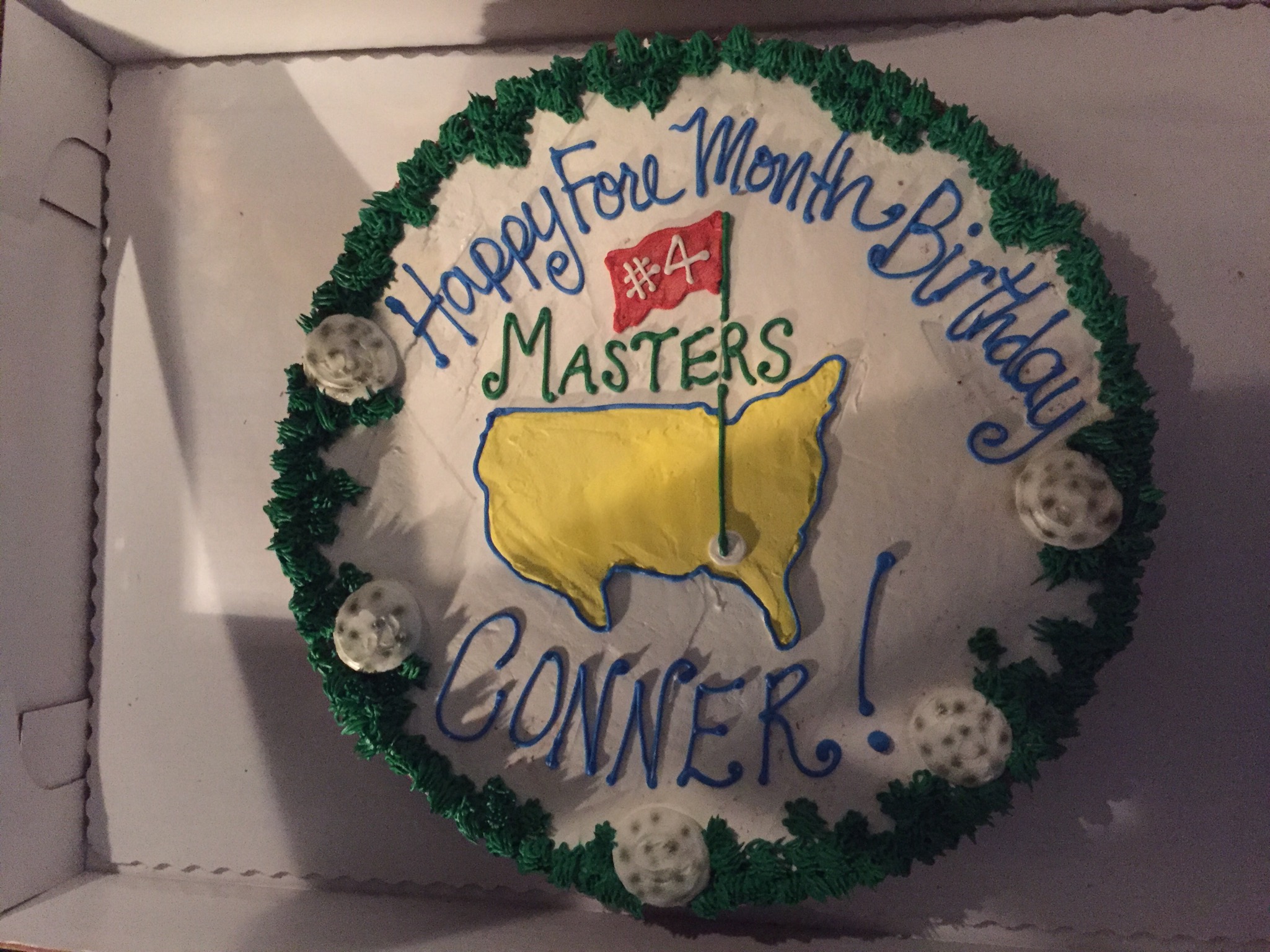
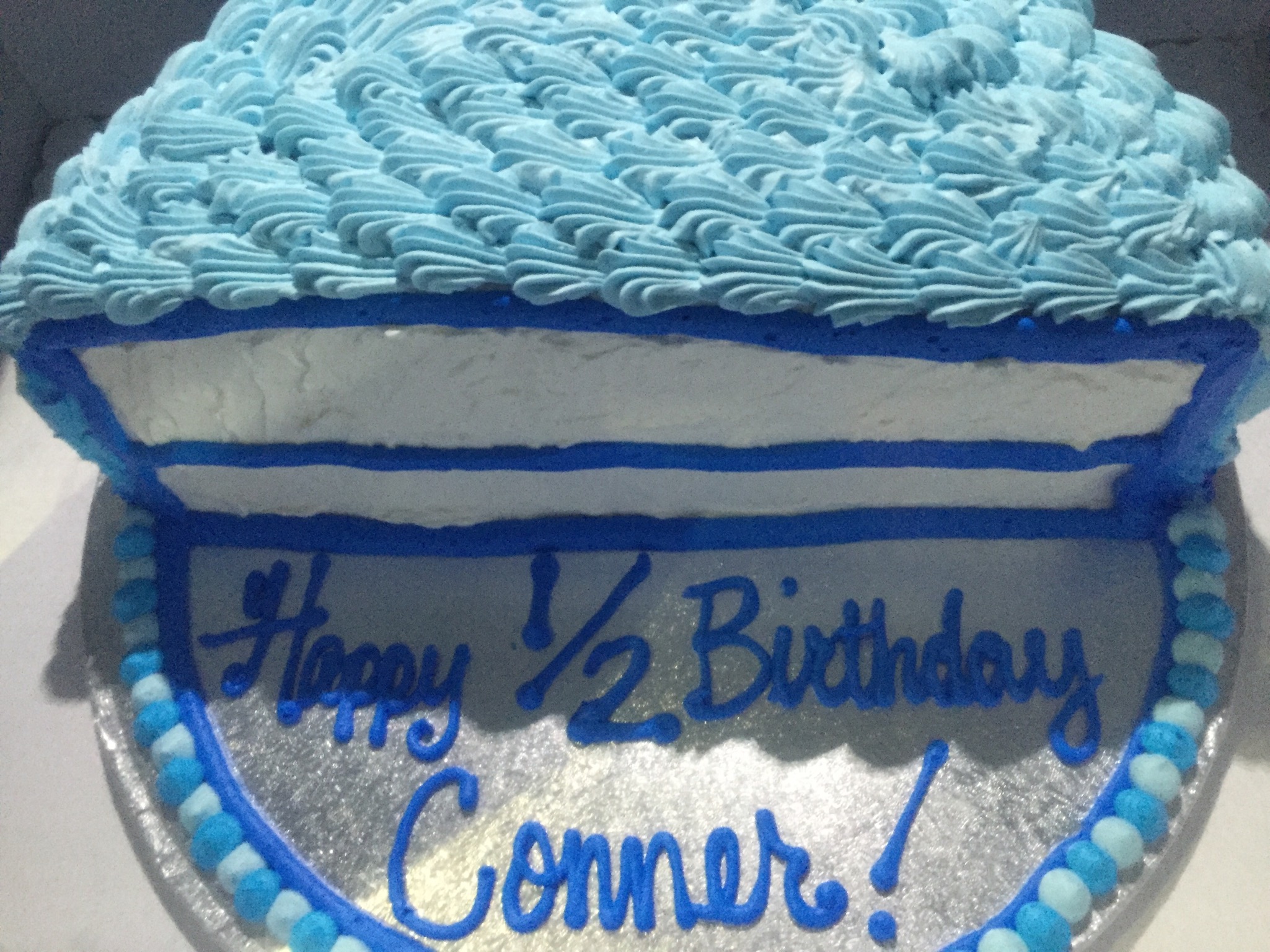
The NICU taught me to celebrate every milestone - big or small. Most importantly I grew to appreciate learning experiences and time with loved ones - especially Con-man.
Conner has some seriously impressive stats from the NICU:
· 194 days in patient in two NICUs
· Hundreds of blood draws and heel sticks (upwards of 8x/day at times)
· Hundreds of breathing treatments (we still do this twice a day)
· Hundreds of X-Rays (we lost count quickly)
· 14+ blood transfusions
· 7+ PICC lines
· 5 head ultrasounds
· 5 abdominal ultrasounds
· 3 bowel surgeries (2 emergent)
· 3 kidney ultrasounds (he has one functioning kidney)
· 1 set of eye injections (Avastin to treat Retinopathy of Prematurity (ROP))
· 1 heart surgery ( Patent Ductus Arteriosis (PDA) ligation at 2 weeks old)
· 1 ambulance ride
· 1 MRI
I often ask myself how we possibly survived 6.5 months in the hospital. I was on autopilot between driving to the NICU, rounds, pumping schedule, Conner’s care times, etc. The only thing I can think of that kept us moving forward is the support of family, friends and NICU staff. We are fortunate enough to have both sides of our immediate families nearby and they were there anytime we needed something and even when we didn’t. Our friends texted support; they knew not to call because the NICU would call if something was going on with Conner when we weren’t there (phone ringing = panic).
Conner with his neonatologist, Dr. Anderson, on discharge day! This was a bitter sweet day for sure.
I couldn’t have picked a better primary Neonatologist for Conner (and us). Craig Anderson, D.O. is without a doubt the biggest and most loyal Oklahoma City Thunder fan you'll ever meet. His love for his job is second only to his love for Stevie Nicks. Our personalities meshed and Dr. Anderson was very upfront with us about Conner's health, which we preferred (even if he used the word "critical" about 97 times the night Conner was admitted). He also brought humor to the NICU and referred to Conner’s room as District 9 (Conner was in room 9 and you have to be a Hunger Games fan to find the humor in that). We had some amazing nurses and respiratory therapists that took care of Conner like he was their own and will remain forever friends. And lastly, I have gained some friendships with other NICU moms that I would not have had otherwise. The bond you form with other parents going through similar circumstances is unmatched.
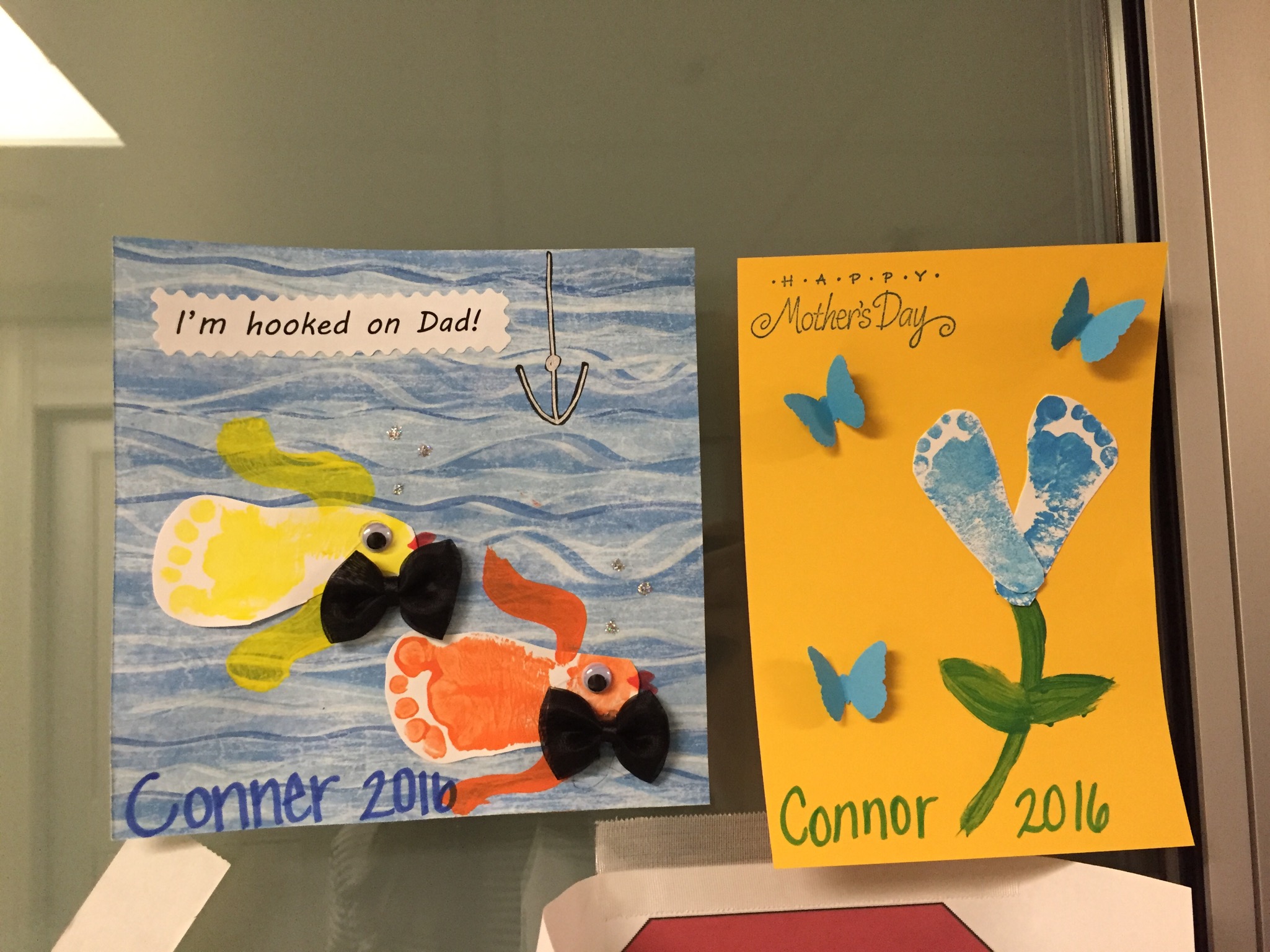
If you're as lucky as we were, you'll have doctors, nurses and respiratory therapists (RTs) that turn into family. You'll have people taking care of your baby AND you. More times than I can count, Conner's team treated us with homemade salsa, cookies, ice cream (to celebrate making it through big days) and so much more. When we weren't there, his nurses made crafts with Conner's ever-growing footprints that decorated his NICU door - they are proudly displayed at home now. Conner was especially spoiled with Oklahoma City Thunder gear, stocking caps and even puffin slippers from Iceland! My favorite gift, hands down, is a race bib from Conner's RT, Paul, that took care of him the night of his first emergency surgery (after he was transferred across town). The weekend following Conner's surgery, Paul ran the Oklahoma City Memorial Marathon and returned to our room with his bib in hand (pictured above). I can't decide what I love more - the message on the bib or the pure kindness of someone that barely knew us.
More NICU Knowledge to Know...
Chronic Lung Disease
Chronic Lung Disease seems to be a given for any micro preemie. Conner was intubated on a ventilator (with and without a jet pump), SiPAP, oxygen (varying flows), at room air, back on oxygen, intubated again...you get the point. More often than not, he was receiving some form of support to breathe. Conner also received countless X-Rays to check the condition of his lungs. He received breathing treatments multiple times a day during most of his NICU stay. In fact, he still gets a breathing treatment twice a day now, but he's progressed to only one inhaler (with a spacer). He was very lucky to not go home on oxygen and we are so thankful that his lungs continue to grow stronger.
Retinopathy of Prematurity (ROP)
ROP is a disease of the eye affecting premature babies, in which oxygen therapy is used on them due to premature development of their lungs. ROP was a concern very early on and continued for months. When he was stable enough, he would receive weekly eye exams to check the retinal blood vessels in his eyes. I will warn you NICU parents out there...the eye exam is not pretty. I wish I was more prepared for seeing my son's eye forced open with a tiny metal clamp. However, it is quick and over before you know it. ROP can be very serious and can cause retinal detachment or even blindness in serious cases. There are three stages of ROP - 1 being the least concerning and 3 being very serious. Treatments include laser surgery and Avastin injections. Conner's eyes were doing okays for a bit, but when his ROP developed into stage 2, he received Avastin injections. Avastin is not a guaranteed treatment, so he was monitored for a few weeks following his injections. Thankfully that treatment did work for Conner.
Conner's eyes would be dilated before his eye exam...he always had more smiles during this time. I wonder what he was seeing!
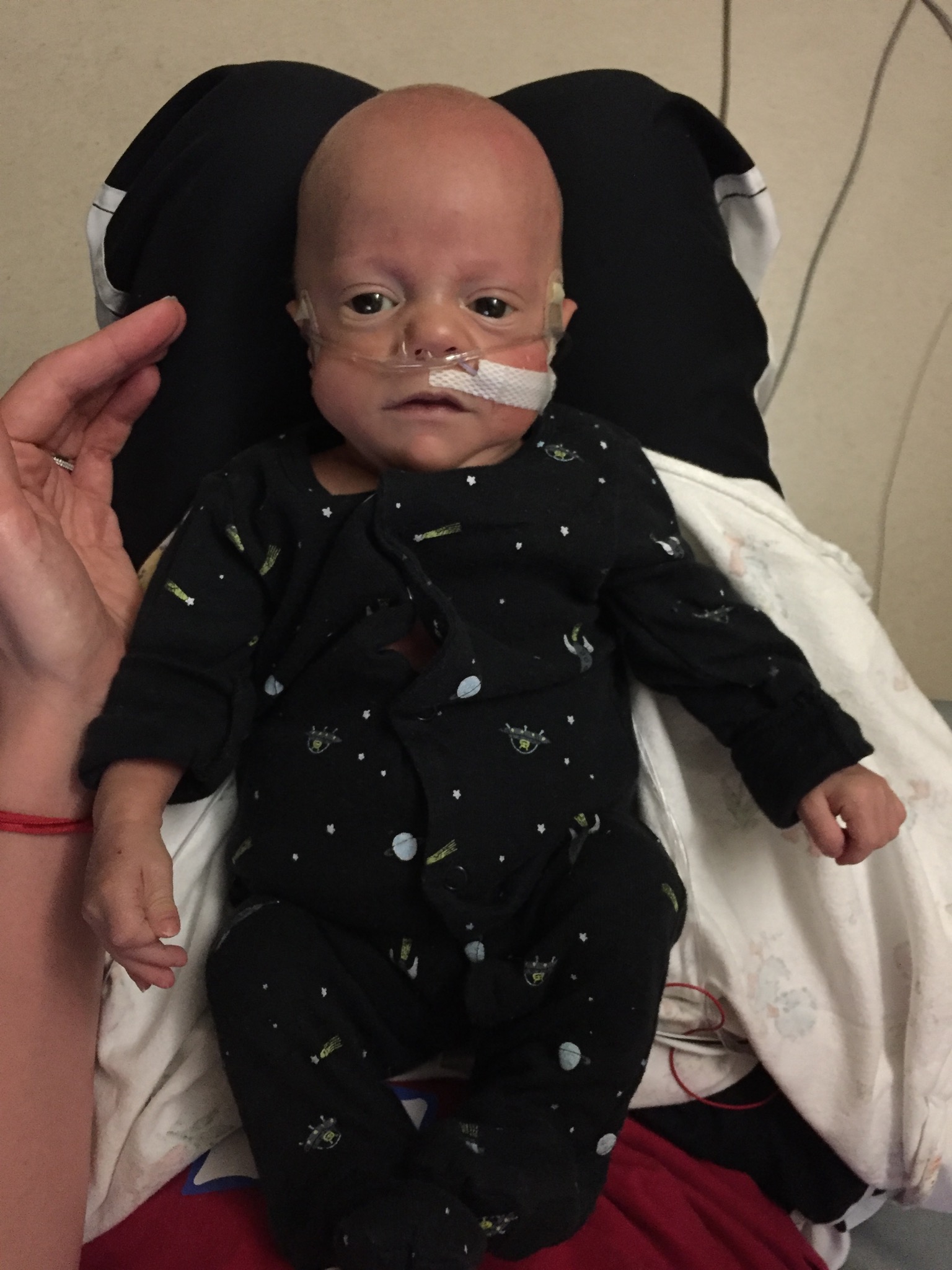
This was taken shortly after Conner's PDA Ligation
Patent Ductus Arteriosis (PDA)
Patent ductus arteriosus (PDA) is a heart problem that's common in premature babies. Before birth, a large artery called the ductus arteriosus lets the blood bypass the lungs because the baby gets its oxygen through the placenta.
The ductus normally closes soon after birth so that blood can travel to the lungs and pick up oxygen. When the ductus does not close properly, it can often lead to lung damage and prolonged reliance on the ventilator. Medication is sometimes used to get the ductus to close, but surgery is often required. Conner did not respond to the medication, so surgery was needed. At two weeks old, our then 1lb 2oz baby underwent open heart surgery. To give you an idea about how tiny he was, to open his ribs to access his heart, an eye lid clamp was used. The decision to proceed with Conner's PDA Ligation was left up to us - a decision I was not prepared to make. Our other choice was to give him more time and hope that it closed on it's own. We Are thankful that the PDA Ligation was successful and that we made the right decision for Conner. Conner's incision was maybe half an inch, but now it spans across most of his back. He can impress just about anyone with his NICU battle wounds!
Necrotizing Enterocolitis (NEC)
If you or someone you know had a very premature baby, then you probably recognize the dreaded term, NEC. It stands for Necrotizing Enterocolitis and it is devastating, for lack of a harsher description. NEC is an intestinal disease that can effect babies (typically premature). It can cause the intestines to become inflamed or in rare cases perforate which will wreak havoc on the tiniest and sickest of babies. That is exactly what it did to Conner. To read more about Conner's NEC and ostomy journey, click here.
Intraventricular hemorrhage (IVH)
Intraventricular hemorrhage (IVH) are commonly referred to as brain bleeds. Babies weighing less than 3lbs have the highest risk for a brain bleed. They usually occur early on in life, but many resolve on their own. More severe ones can lead to cerebral palsy or other problems.
Pumping for a Preemie
Pumping for a preemie is truly hard work. It seems constant and for anyone that has been hooked up to a breast pump, you know it's borderline torcher! I rented a hospital grade pump and strongly encourage anyone else with a preemie to do the same. The NICU provided one-time use bottles to help reduce any germs/contamination and labels to place on each bottle to identify which baby it is for. Conner was strictly bottle fed because we had to add calories boosters to help Conner gain weight. Conner was on prolacta and then human milk fortifier (HMF) when he was too old for prolacta.
I wish I would have started to put my milk in bags sooner. I was able to provide enough for Conner (especially because he was NPO - nothing by mouth - often), so I started to freeze the bottles at home. The bottles took up quite a bit of space and Conner would not get the frozen milk until he came home anyway. We were fortunate enough to have 3 deep freezers from friends and neighbors that were donated to us. I filled all three to the brim and it is one of my greatest accomplishments as pumping was harder than I ever imagined.
Pumping for Conner often felt like the only thing I could do to help him - that acted as my motivation on days I really just wanted to quit.
As you can see, I loved pumping so much, I spent a lot of time documenting it!
You'll never get use to the alarms
In the beginning, every single alarm will bring panic as you stare at the blinking number(s) on the monitor trying to figure out what they mean. You quickly learn what each number means and when you should actually start panicking. However, the fear still overcame me until I could look at the monitor and reassure myself all was well. If you leave the NICU without monitors (like Conner did), it will be very difficult to let go of the comfort that comes with knowing your baby's heart rate and oxygen at all times. Conner was hooked up to a pulse ox while he slept until he was almost two - solely for our comfort.
Beads of Courage
Beads of Courage is a program that provides arts-in-medicine for children with serious illnesses. The beads are a visual reminder of everything children go through during hospital stays. The beads range from birth to discharge and every test, poke and surgery in between. during his 6.5 month NICU stay, Conner has upwards of 1,600 beads. This kid has endured it all. To learn more about Beads of Courage, click here.
Conner and Fenway with all of his beads!
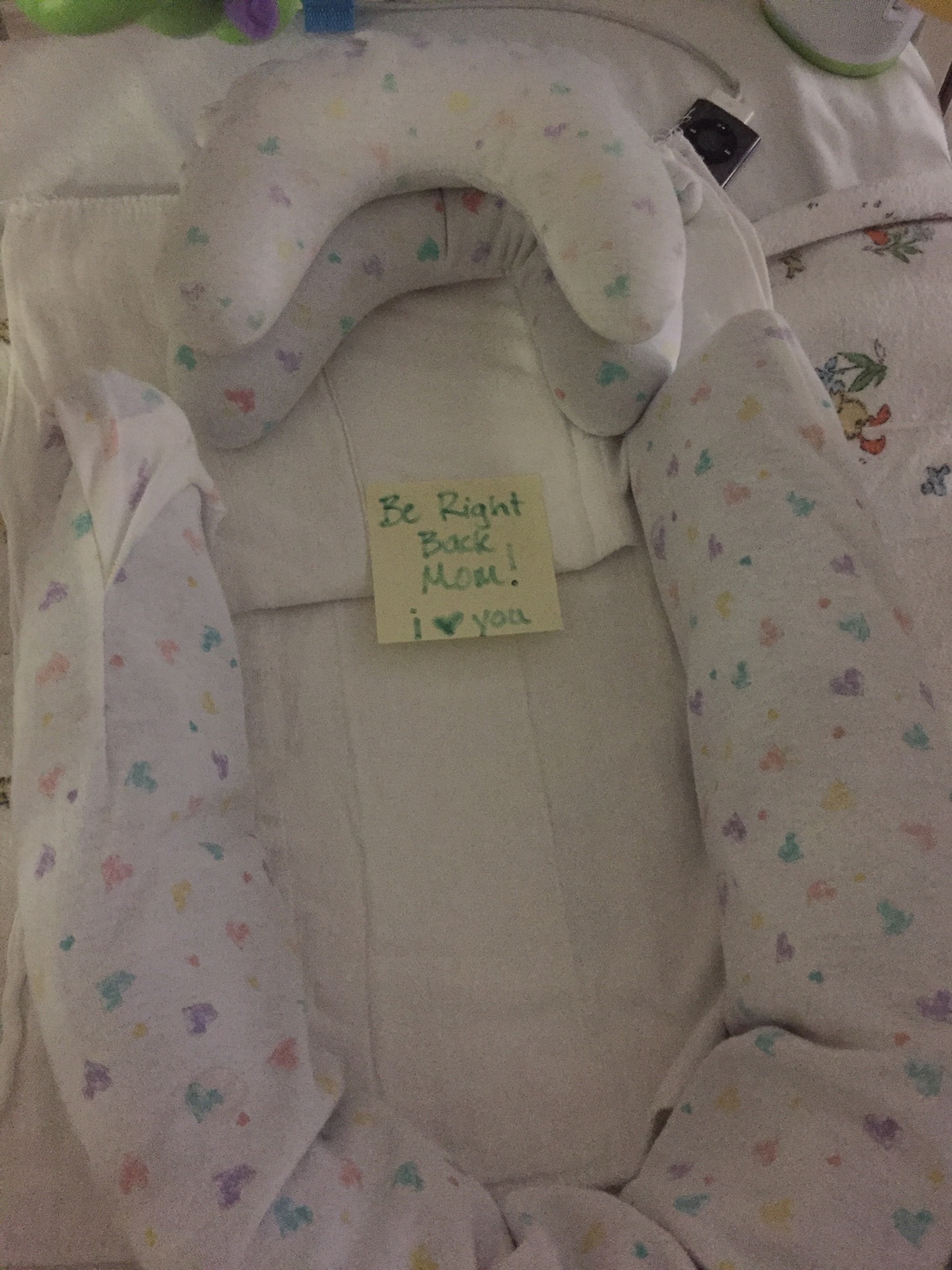
If you're lucky, you'll get awesome nurses who leave you notes from your baby and do footprint crafts!
Picking primary nurses
Primary nurses are ones that you select to care for your child when they are working. The nurses then have to agree to take your baby on as a primary. Check with your NICU/s nurse manager about picking primary nurses for your baby. Picking primary nurses was so helpful for me. Sometimes you bond with a nurse and sometimes the connect just isn't there. I especially appreciated Conner's night nurses because it allowed me to go home to sleep. I would call during my pumps through the night to get updates. Ones that gave me the full report upfront were often my favorites. Thinking of all the questions you wanted answers to while you're half asleep was pretty difficult. We also asked that the neonatologists/nurses NOT call us unless it was very serious. We were there most of the time anyway, but getting a call when we were away was like a punch to the stomach. It didn't happen often.
It's okay to take a break
Taking a break from the NICU is difficult to do, but it will help you in the long run. We rarely took breaks from the hospital the first couple weeks after Conner was born. He was too fragile and we couldn't bear to be more than a few minutes from his room. We spent many nights in Conner's NICU room when he was his sickest. When he was improving and we found night nurses we grew to trust, we were able to go home for the night. I often found myself feeling guilty or worried I'd be judged if I left, but that couldn't be further from the truth. Nurses will encourage you to take a break because they know it will help you! I often took a quick break for lunch and to give our dog, Fenway, some attention. I would then returned back to the NICU until shift change. I liked to be there for the evening shift change to hear the report and to participate in Conner's weigh-ins (nightly weight checks were a big deal - it often dictated some changes for the following day). Everyone is different, so find what works best for you and your family.
You can't prepare for it all
You may think you're prepared for it all, but it's just not possible. You can't prepare yourself for how tiny and fragile your baby might be. You won't be ready for the alarms, medication pumps, ventilator, jet pump or even the phototherapy light. The NICU experience is very overwhelming at first. If you're there long enough it starts to feel more like home than your actual home.